-
Research
Clue to Early Indicator of Type 1 Diabetes Identified
In a recent paper published in Cell Reports, Mayo Clinic scientists found that extracellular vesicles encouraged inflammation of pancreatic beta cells and their environment in mouse and cell culture models. Diabetes is a chronic condition where beta cells of the pancreas produce little to no insulin, which is a hormone that controls how the body processes nutrients in the bloodstream.
In Type 1 diabetes, beta cells are damaged by the body's immune system through chronic inflammation. People with this chronic condition must take insulin daily. There is no cure, and early-detection methods are urgently needed.
"The goal of this study was to look into novel strategies to restore overall beta cell function and health in individuals with Type 1 diabetes," says Naureen Javeed, Ph.D., a Mayo Clinic scientist and lead author on the new publication. "Our strategy was to understand how beta cells facilitate their own demise during progression of Type 1 diabetes and use that knowledge as a potential target of therapeutic intervention and as an early detection biomarker for the disease."

Communication is Key
The researchers suspected that communication between beta cells contributed to cell stress and, ultimately, their failure. Cells must communicate with each other to respond to the constantly shifting situation in the body. To manage this chaos, cells talk to each other chemically, but also by exchanging cellular material.
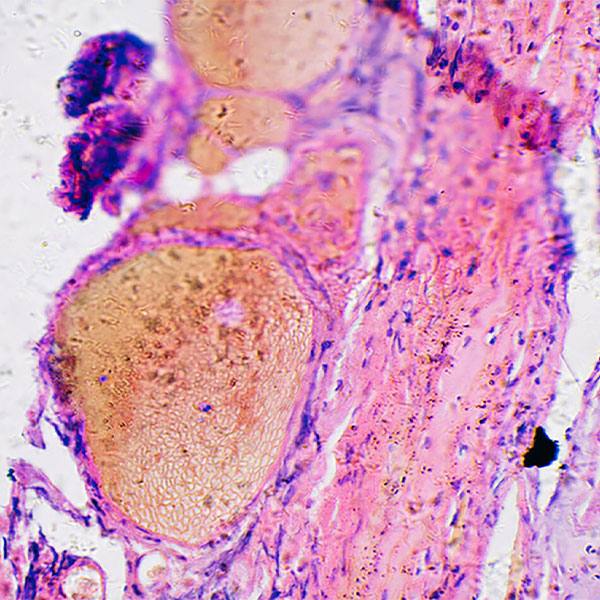
These cellular cargo can consists of proteins, DNA, RNA or lipids, and it can be passively gathered or purposefully packaged in membrane-formed cellular cargo ships called extracellular vesicles. They protect cargo traveling between cells through the hostile intercellular space.
"Several studies in a variety of diseases have found that the content of EVs (extracellular vesicles) becomes altered as the physiological state of the cell changes during disease progression," explains Dr. Javeed. "We decided to exploit this idea by looking at how a proinflammatory environment in a model of Type 1 diabetes alters beta-cell-derived EV cargo and function."
The scientists found that when exposed to inflammatory chemical signals, the extracellular vesicles from the altered beta cells pushed other beta cells to fail and encouraged inflammation in the beta cell environment by calling in T cells and macrophages. Investigating the cargo, the team found a specific signaling chemical ― a protein called CXCL10 ― to be highly abundant. They examined how this protein interacts with beta cells and then blocked it from docking to the cells. When blocked, beta cell function improved. The authors suggest that this cellular conversation takes place early in Type 1 diabetes progression.

"Our results potentially suggest these EVs are involved in the early stages of Type 1 diabetes disease progression rather than at the final stage of beta cell death. This has potential impact on biomarker discovery, as it may be plausible that the packaging of CXCL10 in the EVs could be an early event that precedes Type 1 diabetes diagnosis," says Dr. Javeed.
Based on this data, the researchers received a joint grant from Mayo Clinic's Center for Biomedical Discovery and Mayo Clinic's Center for Clinical and Translational Science to expand their work and determine if CXCL10 expression in extracellular vesicles could be used as an early diagnostic test for Type 1 diabetes. With recent federal funding from the National Institute of Diabetes and Digestive and Kidney Disease, Dr. Javeed also plans to investigate the fundamentals of extracellular vesicle biology as they relate to diabetes development.
"We are excited to make basic science discoveries that can be directly translated to the clinic," says Dr. Javeed. "Extracellular vesicle biology is an emerging topic that Mayo has been very interested in over the past few years, and I am eager to contribute to understanding this field better, particularly in the context of diabetes."
Other authors on the paper are research technologist Tracy Her; Matthew Brown from the Mayo Clinic Graduate School of Biomedical Sciences; Patrick Vanderboom, Ph.D.; Kuntol Rakshit, Ph.D.; Aoife Egan, M.B., B.Ch., Ph.D.; Adrian Vella, M.D., the Earl and Annette McDonough Professor; Ian Lanza, Ph.D.; and Aleksey Matveyenko, Ph.D. ― all from Mayo Clinic. See the full paper in Cell Reports for funding information, including support for Dr. Javeed from the James A. Ruppe Career Development Award in Endocrinology and support from Mayo Clinic's Center for Regenerative Medicine and Mayo Clinic's Center for Biomedical Discovery.