-
Biotherapeutics
Beyond stem cells, regenerative medicine finds exosomes
Exosomes, a new tool in regenerative research, have implications for cardiac and tendon regeneration, wound healing, and incontinence, as well as many other applications.
In the 60 or so years since stem cells were first defined, they've become heralds of a new type of medicine, one that promises to harness the body's healing properties. Stem cells are a sort of cellular blank slate and can be engineered to form any cell in the body. Ones collected from adults can only grow into certain types of tissue or be maintained in a stemlike state.
While a vast storehouse of knowledge on stem cells exists, clinical indications remain elusive. Stem cells are expensive, difficult to transport, and stem cell therapy results are unpredictable. So instead of investigating the actual cell, Mayo researchers are investigating how the cells do their work. Assembled from the Mayo Clinic Van Cleve Cardiac Regenerative Medicine Program, clinicians, and Mayo's business development group, the team is using a new substance linked to stem cells called exosomes, and bringing it to the health care market. While it's not yet known if this product benefits patients, it's a great time to see how a research idea translates into a potential cure.

Stem Cells to Heal the Heart
Atta Behfar, M.D., Ph.D., is a Mayo Clinic cardiologist. As a graduate student at Mayo in the 1990s, he started one of the first stem cell projects in the lab of Andre Terzic, M.D., Ph.D., the Marriott Family Professor of Cardiovascular Research, and the Marriott Family Director, Comprehensive Cardiac Regenerative Medicine for the Center for Regenerative Medicine. The lab was investigating how to use stem cells to regenerate heart muscle after the damage caused by a heart attack.
"In the early 2000s and even up to 2010, our main focus was to take stem cells and maximize their regenerative power," explains Dr. Behfar. They used a type of cell known as mesenchymal stem cells. These cells are collected from the bone marrow or fat. The team manipulated the mesenchymal stem cells to create a heart regeneration cell, called cardiopoietic stem cells, and studied this cell through preclinical and human clinical trials.
"We did a small phase 2 and a large phase 3 trial with the cardiopoietic stem cells, and we saw benefit in patients but not uniform benefit," says Dr. Behfar. Some patients showed marked improvement, while others showed no change at all. In studying the difference between the participants, the team examined every factor, including the stem cells given to each participant.

Not the Speaker, But the Words
Cells exist in an environment that changes second by second, responding to everything that is done, eaten, and experienced, all while communicating information to each other. It is, Dr. Behfar says, chaos.
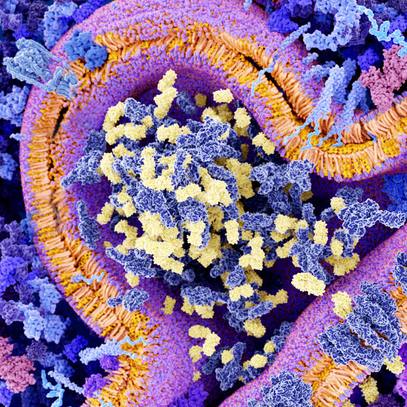
Within this chaos, cells communicate and influence their environment. Skin damage, for example, triggers a call for immune cells and reparative cells to heal the wound. This message for healing is called an extracellular vesicle. Discovery's Edge wrote about vesicles in 2018 in "Shuttling Through Inner Space." Put simply, extracellular vesicles are like space shuttles that protect cargo traveling through hostile intercellular space. Originally thought to be cellular trash bags, these nanoscopic spheres are now getting their due.
"Every cell makes different types of extracellular vesicles in response to different environmental cues," explains Dr. Behfar. "Extracellular vesicles in the body are even more varied than the different types of cells in the body."
While some vesicles are passively released, they also can be purposefully packed and released in the form of exosomes. As Dr. Behfar and team studied the difference between responders and nonresponders to stem cell therapy, they found a crucial difference in the types of exosomes released by highly regenerative stem cells. These are what Dr. Behfar calls "super-regenerative stem cells" that communicated with an exosome message of healing loud enough to cut through the chaos caused by inflammation and lack of blood flow.

Translating Stem Cell Commands
Over the next several years, Drs. Behfar and Terzic, and their team, investigated the cargo of the exosomes. They examined every molecule packaged in the little shuttles and then reverse-engineered exosomes to replicate the effect. It was a huge success but a bittersweet one. Stem cells were the source of the exosomes they engineered. This presented significant challenges to scaling up their finding into a product that could be made and stored for clinical use.
"Depending on how dense stem cells are in a petri dish, what kind of environment they're in, and even the atmospheric pressure influences how they will behave. It is extremely hard to get the cells to secrete the exact type of exosomes we were looking for. The only way to control for that was to have a massive number of identical cells," he says.
But growing stem cells is expensive and can take months. So, any eventual stem cell treatment may also require months to plan and would be costly. They needed something else capable of making the exosomes and some help understanding the future for exosomes as a medical treatment.

Making a Medicine, Not a Research Finding
Mayo Clinic's Center for Regenerative Medicine was established in 2011 to coordinate growing interest in the ways the body could regenerate itself. Mayo also began building a facility to make regenerative medicine projects, like exosomes, that could move into clinical trials. By 2015, Drs. Behfar and Terzic had deciphered the message of healing from the stem cell exosomes. They felt sure it could be a valuable product for a range of situations if they could figure out the best way to make it. For that, they needed help.
In 2013, Mayo Clinic began allowing staff to form startup companies and invested in programs to guide this effort within a scaffolding of comprehensive and robust conflict of interest policies. For advice, Dr. Behfar and team approached Mayo Clinic Ventures, which bridges the Mayo research and practice efforts to translate medical ideas into medical advances for patients. Andrew Danielsen, chair of Mayo Clinic Ventures, explains that they have a process they walk through with the researchers.
"When a researcher comes to us with a new technology, we do an analysis," says Danielsen. "Is this patentable? Is it novel? Will we be able to find a commercialization partner? If no, we thank them and encourage them to come back with their next idea. If it is patentable, or if we're not sure, we file a patent and continue with the process to find a partner to develop a clinical product with our inventors."
With a patent, Danielsen's team can reach out to entrepreneurs, investors and companies to gauge their interest. Many times, it's too early, but the conversation allows Mayo Clinic Ventures to gather valuable information for the researcher on how to proceed.

"The researcher hopefully can complete the additional work to advance the technology," Danielsen says. "If so, we look to find a good commercial partner, and we talk about a license. Then the last piece is getting fair value for this technology for Mayo Clinic."
In the case of the exosomes, Drs. Behfar and Terzic used Mayo's Employee Entrepreneurship Program to start their own company, making the exosomes available for many uses. Instead of using stem cells, the researchers figured out how to use a type of blood cell called platelets as their starting cell. This was a much more accessible and less expensive source. The platelets were put in a tightly controlled environment that caused the cells to make the specific exosomes containing molecules that cut through the chaos and push a message of regeneration.
Along the way, the researchers refined the tests used to identify the target exosomes, which allowed them to define purity versus impurity. In the end, they arrived at a purified exosome product that was sterile, pure and able to be freeze-dried into a powder so that it could remain stable in storage.
"The purified exosome product can sit on the shelf at room temperature for a year and be just as potent," says Dr. Behfar. "Although the focus of the Van Cleve program has always been cardiac regeneration, we suddenly realized that we could truly facilitate soft tissue healing much more broadly." And with an actual product in place, the team expanded beyond their original research.

Wound Healing, Incontinence, Tendon Regeneration and Beyond
So far, Mayo researchers have tested the purified exosome product for a variety of potential uses, with several preclinical studies completed. Working with Steven Moran, M.D., a Mayo Clinic plastic surgeon, the purified exosomes helped skin heal without scarring. Which, Dr. Behfar says, is particularly exciting as a potential treatment for patients.
"Typically, all these technologies cover wounds effectively with the hope that the protective environment would help the body regenerate more effectively. But we've seen so many patients in clinical practice who ultimately still require amputation despite our best efforts," says Dr. Behfar. But what they see with exosomes, he continues, is not just that the wound is closed, but that the blood supply is restored in preclinical studies. Those two findings — blood supply restoration plus wound healing — make the exosome product a potential future therapeutic in cases where amputation is the only option.
In another study led by Chunfeng Zhao, M.D., a Mayo Clinic orthopedic surgeon, the exosome product applied via a patch supported the success of tendon repair. And with John Occhino, M.D., a Mayo Clinic urogynecologist, the exosome product was investigated for vaginal wound repair after injury from mesh exposure. Another area of current investigation, with Emanuel Trabuco, M.D., a Mayo Clinic urogynecologist, is urinary stress incontinence, where the bladder leaks urine when under pressure — like when a person laughs or coughs.

"We know that it is caused by a deficit of the skeletal muscle, which prevents the urethra from releasing urine," says Dr. Behfar.
These muscles in the pelvic floor are weakened due to damage from childbirth or during some procedures, such as prostate surgery. Drs. Behfar and Trabuco are using the exosomes to see if they can strengthen the pelvic floor muscles by telling the body to make new muscle tissue.
Wound healing, cardiac and tendon regeneration, incontinence - and that's just what's going on a Mayo. While these are early investigations, providing a way for research ideas to reach the health care market helps expand the potential of an idea. The startup can focus on moving the exosome product through the regulatory approval process, while other companies licensed to use the exosomes pursue different uses. It works well because there are many good research ideas, but without teamwork and a framework for bringing them into clinical care, the message can get lost in the chaotic cacophony of daily life.
"I think this is a quintessential Mayo Clinic story," says Dr. Behfar. "We have a team of collaborators, and we are all working for the betterment of patient care across multiple departments. Whether we help our collaborators succeed, or we succeed in cardiac regeneration, the main objective is to provide new hope to patients without good treatment options. And that is Mayo's mission."
— Sara Tiner, July 2021
- To read about extracellular vesicles, click through to "Shuttling Through Inner Space."
- For more about exosomes and wound healing, head over to the Regenerative Medicine Blog.
- For regenerative medicine approaches to incontinence, read "Focus on Women's Health."