-
Biotherapeutics
Stem cells in space: A new frontier in regenerative medicine training

A Mayo Clinic graduate student is looking to the stars as a new way to advance regenerative therapies for cancer. Rawan Al-Kharboosh, a Ph.D. candidate at Mayo Clinic’s Florida campus, is investigating how stromal vascular fraction stem (SVF) cells react in microgravity and if that may be applied to fight the most deadly type of brain cancer — glioblastoma. SVF cells are a type of cells with the potential to regenerate tissue.
Treatment of the glioblastoma has seen little improvement in outcome in the past decades, with a dismal prognosis and a devastating median survival of 14.6 months. Despite vigorous treatment combinations of surgery, chemotherapy and radiation, there is nearly a 100% recurrence rate. The microscopic cells left behind after surgery – the ones that are not seen on an MRI – are responsible for its resistance and ultimate relapse.
Al-Kharboosh is enrolled in the neuroscience track of Mayo's Ph.D. program and is a scholar in the Regenerative Sciences Training Program (RSTP), supported by the Mayo Clinic Center for Regenerative Medicine. The program, led by Jennifer Westendorf, Ph.D., and administered through the Mayo Clinic Graduate School of Biomedical Sciences, is designed to prepare the next generation of researchers and advance regenerative sciences into clinical practice.
In January, Al-Kharboosh’s research cells are scheduled to rocket on a suborbital flight, in which it reaches the point of weightlessness but remains below the altitude where it can orbit Earth. She will examine how microgravity affects SVF cells derived from human fat (adipose tissue), and if stem cells can be engineered in a way to allow for same-day engineering. The results of her experiment may shed light on whether SVF can be engineered in microgravity and if these cells could be reintroduced to the brain during cancer surgery to promote healing.
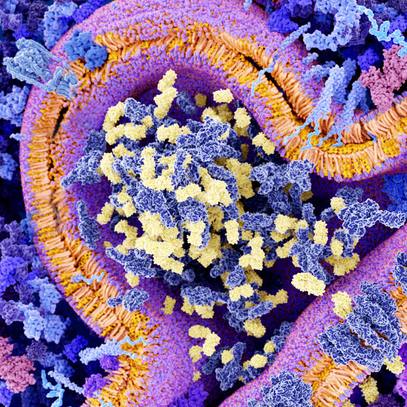
“We isolate stromal vascular fraction derived from human fat (adipose) tissue directly from patients in the operating room,” says Al-Kharboosh. “We are exploring the possibility of engineering these cells with nanoparticles to target and combat brain cancer by releasing a therapeutic cargo.”
When returned to the patient, engineered adipose-derived cells act as vehicles to target and combat the cancer cells. Right now, this is done in a laboratory setting with the cells adhering to and growing on a plastic plate. It takes a few hours for the cells to adhere to the plastic and even longer for their growth. Al-Kharboosh was curious to find ways in which the modified cells could be engineered in suspension rather than on a plate.
Engineering cells in suspension avoids laboratory processing, is less expensive, more accessible and explores a platform where “same-day” engineering is possible and could be done by a physician in the operating room while patient is at the bedside.

"Rawan’s work is extraordinary. In some ways revolutionary," says Al-Kharboosh's mentor, Alfredo Quinones-Hinojosa, M.D., a neurosurgeon on Mayo Clinic's Florida campus. "She is helping to find potential therapies — and maybe one day cures — for patients with cancer and other neurological diseases. It is highly risky, but it also could be highly rewarding."
Rawan says the students in the Regenerative Sciences Training Program meet during class seminars and journal clubs to discuss their research. They provide input on each other’s work and discuss ways to navigate the discovery, translation and application of regenerative research and therapeutics, and the more difficult topics of regulatory, political and ethical considerations of regenerative medicine and stem cells.
Mayo Clinic Center for Regenerative Medicine supports 17 students in the RSTP program, including Al-Kharboosh. The center selects student who will go on to careers that advance the regenerative sciences field and bring new regenerative therapies to patients. Al-Kharboosh says her dream is to be the CEO of a large biotech company that discovers and develops regenerative products for patients.
Read more about Rawan Al-Kharboosh and her research in Discovery’s Edge.