-
Cancer
Lymphoma Treatment Questioned In Pharmacy Research Study
Physicians who treat patients with cancer of the central nervous system got some new information that may help their patients with lymphoma. The findings were recently published in Supportive Care in Cancer.
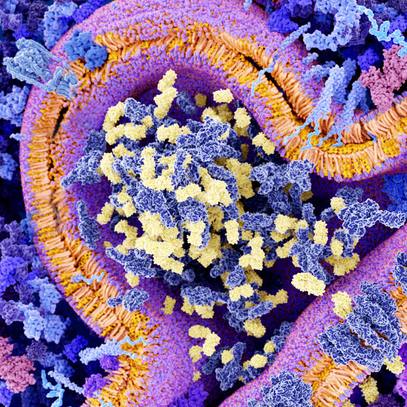
Methotrexate is a drug that can pass though the blood-brain barrier, so is an integral component of chemotherapy for patients with lymphoma involving the central nervous system. However, high-dose methotrexate blocks the body from using folate and can cause a variety of toxicities in cells and organs, including acute kidney injury in up to 30% of patients due to severe folate depletion. Leucovorin, which acts similarly to folic acid, is given 24 hours after high-dose methotrexate to counter this effect. To manage kidney injury, clinicians monitor kidney function, as well as methotrexate concentration — if the drug's concentration increases, it's a sign that the patient's kidneys are not properly eliminating the drug.
The study was undertaken because no one knew whether proactive high doses of leucovorin would benefit patients who previously experienced dangerous methotrexate buildup or kidney injury. The researchers wanted to determine if high-dose leucovorin rescue was more effective than standard leucovorin when used during a sequential course of high-dose methotrexate treatments. They examined the records of 321 patients who received a total of 1,558 high-dose methotrexate doses. Of these, 265 received more than one dose and were included in the analysis.
They found that proactively giving high doses of leucovorin rescue did not appear to lessen the likelihood of kidney injury. In fact, it seemed that patients who experienced an elevated concentration of methotrexate and received high-dose leucovorin rescue were more likely to have another episode of elevated concentration. Additionally, acute kidney injury with a previous dose did not lead to elevated methotrexate levels following the next dose.
The investigators concluded that an increase in the dose of leucovorin, based on each patient’s case and what the physician expected would help the patient, did not predict improved safety outcomes at the level of the kidney. However, they did note the possible benefits on other systemic toxicities that requires further research.
This study was led by Jason Barreto, Pharm.D., with senior author Kern Health Care Delivery Scholar alumna Carrie Thompson, M.D., Hematology; and included other colleagues from Hematology; Pharmacy — including another Kern scholar alumna Erin Barreto, Pharm.D.; as well as Quantitative Health Sciences; and Nephrology and Hypertension.
See the publication on the journal website for a full list of authors and funding agencies, including Mayo Clinic's Center for Clinical and Translational Science, as well as competing interest disclosures.