-
Cancer
Discovery’s Edge: Cleaning up cancer
Immunotherapy offers new drugs and drug delivery to help the body's "janitor" with its job.
The response of the immune system to cancer is complicated.
Understanding it requires research from the basic scientist to the observation of the seasoned clinician.
“It’s turning out the science is so complicated that it has to be a team effort to get from A to Z,” says Larry Pease, Ph.D., program director of the Cancer Immunology and Immunotherapy Program at the Mayo Clinic Cancer Center. “A very important concept in cancer research is the balance between the discovery element and the application element,” he says.
Large integrated research and treatment centers, such as Mayo Clinic, are especially well suited to making the discoveries needed to advance knowledge and treatments.

“We’re trying to bring all these folks together because each one of them has a piece of the puzzle,” says Dr. Pease. “Once they start talking to each other, then we start to make progress. You have to be able to support the people who are doing the discovery work, you need to be able to support and provide resources to the people who work with patients, and then you need to have this conversation going back and forth so we take discoveries and translate them to the patient.”
Advancing Patient Care
Many of us live with the beginnings of cancer. We just don’t know it. We don’t have a diagnosis. We don’t have symptoms. But day by day, subtle mutations creep into our cells, the beginnings of potentially lethal tumors.
Yet the tumors never take root and grow. Why?
Because our ever-vigilant immune system identifies the mutations, mobilizes an army of antibodies and leucocytes, destroys the malignant cells, and sweeps them from the body.
Occasionally, our immune system fails to detect the intruding malignancies. Or it's simply too weak to destroy them. Then the stage is set for cancer. “We live in a messy world,” says Svetomir Markovic, M.D., Ph.D., a Mayo Clinic melanoma specialist and researcher. “The problem is sometimes the janitor gets tired and stops cleaning it up.”
Scientists at Mayo Clinic (and many other research institutions) are working to get the janitor back on the job. And one way that happens is by improving the drugs, called chemotherapy, that help destroy cancer cells.
Concentrating the chemo
Antibodies are proteins that chemically bind to molecules called antigens that are produced by invaders. Our bodies produce antibodies in response to an infection or cancer.

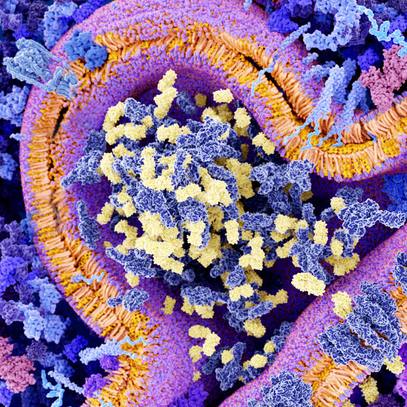
Dr. Markovic is using an engineered antibody to guide an established cancer drug to melanoma tumors. Dr. Markovic, whose background is biochemistry, packs several hundred of these antibodies around a molecule of the cancer drug nanoparticle albumin-bound paclitaxel or nab-paclitaxel. The result, at a scale that can be seen only with an electron microscope, resembles a sea urchin with the cancer drug at the center. The nab-paclitaxel circulates through blood and lymph until the antibodies recognize and latch onto a cancer antigen — like a burr sticking to your pant leg. “Then the whole thing falls apart and releases the drug,” says Dr. Markovic.
By carrying the chemo to the tumor this guided treatment can increase the concentration of the drug where it is needed — in the tumor — while reducing the total dose and side effects to the patient. “If I can truly deliver the lethal hit in the tumor, this may potentially completely destroy it,” says Dr. Markovic.
He is making more antibodies — one for lymphoma and a 2.0 version for melanoma. In the future, he anticipates that these antibodies may carry any of several drugs to the tumor site. It may not even be necessary to know where the tumor is, says Dr. Markovic. “Just target whatever you want. How cool would that be?”
But drug efficacy may be related to more than just powerful drugs. Time has to be on the patient’s side.
Timing is Everything
The body’s fight against cancer ebbs and flows. Fluctuations in immune response are probably caused by the tug of war between the immune system and cancer, says Mayo oncologist and melanoma researcher Roxana Dronca, M.D. Melanoma patients, she says, “live in a state of chronic inflammation. Constantly the immune system tries to mount a

response against the tumor.” But the tumor manufactures chemical signals to quell the response. “The immunity goes up. The tumor counteracts and the immunity goes down.”
By administering drugs at the same time as the body’s strongest immune response, Dr. Dronca hopes to time the therapy to get the best result.
By taking daily blood samples of 29 patients with metastatic melanoma, Dr. Dronca was able to discern immunity cycles that ranged from four to seven days, depending on the patient. She and colleagues were able to administer the chemotherapy drug temozolomide in line with the phases. Says Dr. Dronca, “We found that when we were able to time it right, those patients did a lot better. Some of them actually had complete responses.”
Synergy Within the Mayo Model of Cancer Care
Though the role of the immune system in cancer has long been recognized, it’s only in the last decade or so that scientists have been able to understand at a molecular level how the immune system interacts with cancer before, during, and after treatment.
“Compared to something like chemotherapy, this field is young,” says Allan Dietz, Ph.D., co-director of Mayo Clinic’s Human Cell Therapy Lab. “We’re just learning how best to manipulate the system.”
Immunotherapy advances, discovery-by-discovery at all levels, from basic research to bedside, where doctors “are desperate to do something for their patients and they’re willing to work extra hours to try to figure out new ways to help their folks,” says Dr. Larry Pease.
Cancer, Hiding in Plain Sight
Dr. Pease is one of the basic scientists who try to better understand how the body detects and fights invading cells. The process goes something like this.
Cancer tumor cells, like many other foreign organisms in the body, produce molecules called antigens that have the ability to distinguish cancer cells from the body’s normal cells. These antigens are scooped up by dendritic cells, the immune system’s sentinels. Suspicious antigens are ferried to the body’s lymph nodes where they “educate” the immune system to the threat. Specialized white blood cells, including T cells and “natural killer cells” attack and destroy tumor cells. Some T cells also activate B cells (another specialized white blood cell), which produce proteins known as antibodies that chemically bind to the antigens to neutralize their target or tag it for clean up by other components of the immune system.
Cancer has evolved to evade the body’s immune response. Because tumor cells are our very own cells, the immune system may not recognize them as a threat. Says Dr. Pease, “We have very strong mechanisms of tolerance to prevent ourselves from attacking our own body. So the idea has been that cancers are so much like ourselves that the immune system can’t see them.”

Second, the cancer cells may be producing their own signaling molecules that tell the immune system to call off the attack. “The cancers are co-opting or enhancing this negative regulatory network, which the immune system uses normally to control immunity,” says Dr. Pease. “As immunity ramps up, there are natural mechanisms to turn it back down. Cancers are loaded up with these negative regulators.”
So immunotherapy researchers have two big challenges: strengthen the immune response to recognize and attack cancer; and keep the immune system on high alert, even as the cancer cells struggle to dial down the response.
These are not new challenges. Doctors have long suspected a relationship between cancer and immune response. In 1891 Dr. William Coley at New York Cancer Hospital (now part of the Memorial Sloan-Kettering Cancer Center) injected bacteria into a cancer tumor. The bacteria stimulated the patient’s immune system, and the tumor shrank.
“This is when the field started,” says Mayo oncologist Svetomir Markovic, M.D., Ph.D. And the goal remains much the same. “If we can call attention of the immune system to where the cancer is, the body’s immune defenses will sort of jump on and do their thing — go and destroy the target,” he says. “Since that time, people have tried to turn the immune system on to fight cancer every which way from Tuesday.”
Immunotherapy has advanced far beyond pumping germs into tumors. In the last decade, in particular, researchers have turned detailed knowledge of biology and chemistry in the immune system and tumor environment into a variety of immunotherapy approaches, many of which are progressing from the lab to clinical trials and even into practice.
T Cell Therapy: Building a Bigger Army of Janitors
One approach taken by Keith Knutson, Ph.D., director of the Mayo Clinic Ovarian Cancer Immunotherapy Program, is to remove T cells, which are already trained to clean up cancer, and multiply them into a more numerous force.

Dr. Knutson removes some of a patient’s T cells and greatly increases their numbers in the lab. “It has to be done in an extremely clean environment that minimizes contamination so that you’re not giving something really bad to the patient,” says Dr. Knutson.
“By growing T cells outside the body, you can grow more.” He says he hopes to sidestep cancer’s ability to shut down the immune response by reintroducing T cells into a patient by the trillions. Dr. Knutson anticipates being able to “shrink bulky tumors once they have formed,” even if they are inaccessible. “Sometimes they’re in the bone or in the brain. You can’t get to them.”
Dr. Knutson has focused on breast and ovarian tumors, “but these kinds of strategies could potentially be used as well in other cancers.” Similar work is being done with melanoma and renal cancer. Dr. Knutson anticipates at least a couple of years before the technique is ready for clinical trials. But this is not the only hope for cancer treatment. Dr. Knutson is also developing a cancer vaccine.
Sensitizing the immune system: cancer vaccines
Dr. Knutson’s vaccine hopes are aimed at fighting recurrences of triple negative breast cancer, a disease fatal in about 35-40 percent of cases. Last fall, his team was awarded a $13.3 million grant from the U.S. Department of Defense for a phase 2 trial involving 280 patients with triple-negative breast cancer.
Just as common childhood vaccines prime the growing immune system to fight polio or measles, cancer vaccines sensitize the immune system to the appearance of cancer tissue. Dr. Knutson’s vaccine heightens the body’s response to folate receptor alpha, a protein that has very limited expression in the body but is common in a variety of triple-negative breast cancers, where it is produced by the tumor.

“Our vaccine is designed to stimulate T cells that can infiltrate into the tumor and attack it,” says Dr. Knutson. He anticipates vaccinating patients after they complete treatment (when, it is hoped, they are cancer free). The idea is to boost T cell activity and mop up any residual cancer. Says Dr. Knutson, “If the tumor starts to come back, you’ll have primed T cells ready to attack it.”
In a similar approach, Dr. Allan Dietz trains a patient’s dendritic cells to recognize several different chemical signals of an invading cancer. Dendritic cells “are the sentinels of immunity,” says Dr. Dietz. “They are responsible for detecting problems, and stimulating and then mounting the appropriate immune response totake care of it. They can educate your immune response to tell it what to go fight.”
In clinical trials, Dr. Dietz collects a patient’s cells and cultures them in the lab. “We’ll basically drop pieces of tumor into those cultures. Then we take those cells and we re-inject them back into the patient, in some cases 10 or 15 times. That stimulates and directs the immune response to go against that tumor.”
But in some cases recognition isn’t the problem. Cancer cells can produce chemicals that decrease immune response. And scientists are having a great deal of luck combating that cancer tactic as well.
Releasing the brake: checkpoint inhibitors
A major target of research has been the ability of cancers to call off the immune response before the job is done. Haidong Dong, M.D., Ph.D., immunology researcher at Mayo Clinic, was involved in the discovery of one of the molecular mechanisms — called a “checkpoint” — that tumors employ to hide from the immune janitors.

Dr. Dong was working under the direction of principal investigator Lieping Chen, M.D., Ph.D., (now at Yale University), when Dr. Chen’s laboratory discovered that when the immune system produced the cancer-fighting protein interferon gamma, the tumor cells produced the B7-H1 molecule to turn off the immune response. The molecule (now known as PD-L1) binds to a receptor on the activated T cell (known as PD-1). “And that turns off the T cell response,” says Dr. Dong. By introducing PD-L1 antibody to literally jam up the connection between PD-1 and PD-L1 — a so-called “checkpoint inhibitor” — “then the T cells can kill the tumor again,” says Dr. Dong. The discovery was published in Nature Medicine in 2002. “It was very, very exciting.”
Following the Mayo Clinic discovery, researchers have scrambled to find suitable checkpoint inhibitors to block the PD-1/PD-L1 interaction and allow the immune system to continue fighting cancer tumors. Treatment is sometimes called a “checkpoint blockade.” Early trials are promising — so promising that the U.S. Food and Drug Administration has recently approved the checkpoint inhibitor pembrolizumab for the treatment of advanced melanoma and lung cancer, and nivolumab for melanoma, lung cancer, and metastatic kidney cancer. And approval for more types of cancer may be on the way.
Stephen Ansell, M.D., Ph.D., a specialist in lymphoma at the Mayo Clinic Cancer Center,

has investigated the use of these checkpoint inhibitors in treating patients with Hodgkin’s lymphoma. In a study published in the New England Journal of Medicine, Dr. Ansell and co-authors reported that the PD-1–blocking antibody nivolumab was in fact effective in treating a small group of patients with Hodgkin’s lymphoma who had not responded to conventional treatment or whose cancer had returned. Of 23 study patients, 20 responded and saw their tumors shrink. In some cases, tumors disappeared.
So far, says Dr. Ansell, none of the checkpoint inhibitors has been approved for lymphoma. But with the high response rate in his study, the FDA has given the treatment “breakthrough” status. “It won’t be long where more standard approaches will include the use of an immune checkpoint inhibitor for certain kinds of lymphomas,” says Dr. Ansell.
As with many of Mayo’s research approaches, multiple avenues of inquiry will continue to be pursued in immunotherapy until the unmet needs of patients are met. Check back to Discovery’s Edge for updates on these and other cancer research studies.
- Greg Breining, March 24, 2017