-
Discovery Science
Discovery’s Edge: Moments of Discovery
Curiosity, unconventional thinking, and random chance drive research into new drugs for the treatment of kidney disease.
Granulomatosis with polyangiitis—yes, it’s a mouthful. It’s also a rare disease, afflicting as few as two in 100,000 people. It’s so uncommon a general practitioner might not recognize it. Says Fernando C. Fervenza, M.D., Ph.D., a Mayo Clinic nephrologist. “A lot of physicians down in the community are probably going to see one case in their lifetime.”
But granulomatosis can be deadly. The body’s immune system attacks itself, causing inflammation of small blood vessels, a condition known as vasculitis. And vasculitis can damage sinuses, lungs, kidneys, eyes, ears, skin, nerves, and joints. Until the 1960s “basically it was fatal,” says Dr. Fervenza, who is often called in on such cases when vasculitis inflames the millions of vessels that populate the kidneys.

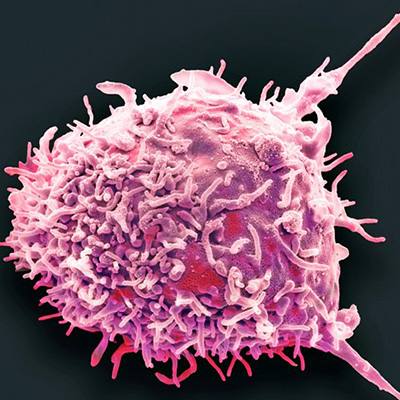
Then came a drug called cyclophosphamide, which suppressed the white blood cells that multiplied to mount the body’s immune response. Cyclophosphamide tempered the body’s attempts to attack itself. “That was a revolution to treatment,” says Dr. Fervenza. An 80 percent mortality rate at one year turned to an 80 percent survival rate.
Yet there was a downside. Cyclophosphamide is toxic. Up to 20 percent of patients either don’t respond to treatment or can’t survive it. “Could we get better results,” Dr. Fervenza asked, “with another drug?” Other doctors wondered the same.
The pervasive nature of vasculitis cases brought Dr. Fervenza together with Ulrich Specks, M.D., the chair of Mayo’s Division of Pulmonary and Critical Care Medicine. “This is a multisystem disorder,” says Dr. Specks. “I would take care of their lung disease, and he would take care of their renal disease, and we would decide on the immunosuppressive therapy together.”
The patient without options
That is exactly what happened with a granulomatosis patient who had been treated with cyclophosphamide but relapsed four years later. When Dr. Specks first saw the patient in 1998 he complained of headaches, scalp tenderness, and large-joint pain. He was treated with cyclophosphamide. While his vasculitis abated, the patient became anemic, probably from the drug itself. Six weeks later he returned to Mayo Clinic with more joint aches, malaise, chills, night sweats, low-grade fever, an inflamed eye, microscopic traces of blood in his urine, a nodule in his lung, and failing kidneys.
He was dying but could take no more cyclophosphamide, the only drug known to put him into remission. Says Dr. Specks. “So then the question is what other agents are there?”
Dr. Specks made his rounds with residents and fellows in tow. After visiting the vasculitis patient, Dr. Specks told the team that cyclophosphamide suppresses the body’s B cells, which seem to play a key role in the possibly fatal autoimmune reaction. That’s when he heard from “one very bright resident at the time” — Marie C. Hogan, M.D., Ph.D., a nephrologist from Ireland.

Dr. Hogan (now on staff at Mayo Clinic) mentioned that a new drug, rituximab, was used to target B cells in patients with lymphoma. As a nephrologist, she was familiar with the use of similar drugs to suppress immune reactions in kidney transplant patients. In fact, at Mayo Clinic she had infused rituximab as an experimental drug in a patient with breast cancer. Back in Dublin, she had seen the drug administered to patients with kidney involvement and had noted its mild side effects compared with cyclophosphamide. She suspected that this drug would selectively target the B cells involved in this form of vasculitis. Might rituximab help the granulomatosis patient? she asked Dr. Specks.
The question sent Dr. Specks to research the drug. Rituximab, he discovered, had recently been licensed by the U.S. Food and Drug Administration to treat B-cell lymphoma. Rituximab attacked the B cells and effectively eliminated them. Unlike the older drug, cyclophosphamide, rituximab seemed to have little effect on the rest of the immune system. Nor did it seem to cause many serious side effects.
“It was an off-label use of a drug that was on the market,” says Dr. Specks. “I put one and one together and we said maybe this is a good alternative for this patient. Why don’t we try this on a compassionate use basis?” Compassionate use is a bit of a medical euphemism that means, this treatment is unproven but you have nothing to lose. Says Dr. Specks, “I discussed this with this patient in detail and he went for it.”
The patient tolerated the experimental treatment without significant side effects. After a second treatment, he went into remission.
Team research has huge impacts
The case of the gravely ill vasculitis patient offered an illuminating case study in collaboration. Dr. Hogan’s off-hand suggestion led Dr. Specks, Dr. Fervenza, and several other researchers (including Dr. Hogan) on a long series of studies and productive papers—and a new and safer treatment for several kinds of vasculitis.
Collaboration is a mysterious alchemy. Hard work and luck. Professional relationships and friendships. Deliberate study and random moments. Dialog between clinical and research. “How many hours do you have?” Dr. Specks asks, as he begins to explain what makes for effective collaboration in research. “That is probably the most difficult question that anybody could ask.”
Dr. Specks and Dr. Fervenza are both physicians and researchers. Dr. Specks is the principal investigator for the Vasculitis Clinical Research Consortium, sponsored by the National Institutes of Health. Dr. Fervenza is the director of the Nephrology Collaborative Group. Over the years, they developed a special relationship with one another, leading to research projects together.
Dr. Fervenza still speaks in a broad Brazilian accent. He is self effacing and chatty. He left Brazil for medical school in England, including time at Oxford. Back in Brazil, he found little use for his specialized training. He came to the United States on a fellowship at Stanford, but had to do a residency again to become eligible to take his boards. That is how he came to Mayo Clinic and met Dr. Specks, who had received his medical degree from the University of Bonn. Dr. Fervenza saw Dr. Specks as a mentor.
After his residency, Dr. Fervenza was hired to develop Mayo’s glomerulonephritis treatment. He and Dr. Specks continued to see some of the same patients, especially when the disease was some form of vasculitis.
Clinical practice often triggers research, says Dr. Specks. “The research questions have always come from patient observations and from problems that arose from not being able to help the patient the way we would have liked to,” he says. “How can we do better?”

Answering that question drove both men to collaborate with each other and a wide range of other investigators to learn more about using rituximab as a vasculitis treatment. Use in small groups proved encouraging. Next was a study of nearly 200 vasculitis patients in nine different medical centers, published in 2010 in the New England Journal of Medicine. This huge study confirmed that rituximab was every bit as effective as conventional treatment. A flurry of later papers further parsed the data obtained in the big multicenter study. Says Dr. Specks, “If you design one good experiment, it’s the gift keeps on giving.”
The studies demonstrated that rituximab effectively controlled vasculitis, oftentimes better than the old drug cyclophosphamide, and was well tolerated by patients. In 2011, the FDA approved rituximab for two forms of vasculitis.
Research continues into the use of rituximab to treat different forms of vasculitis, and into new drugs or new uses of existing drugs that are even more focused in their effects than rituximab is—“drugs that only do what is necessary to affect the mechanism that leads to the relapse,” says Dr. Specks. “That’s ultimately the goal.”
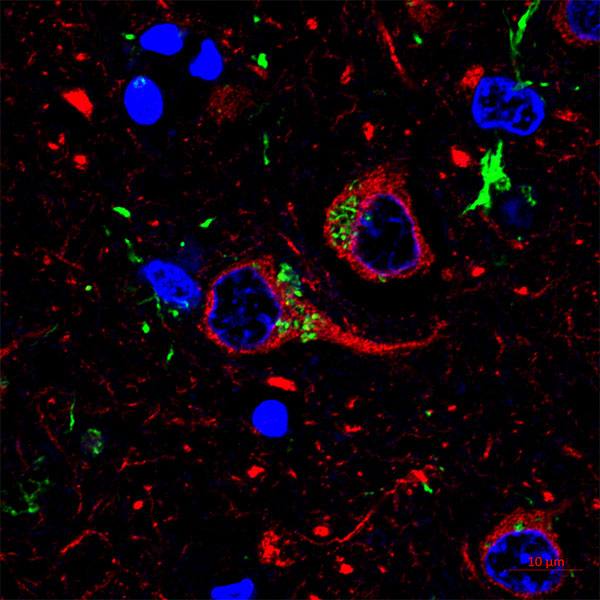
Drugs aren’t the only focus of vasculitis research. Perhaps the most compelling question is this, says Dr. Specks—“How can we identify the patient that will relapse down the road once the diagnosis has been established and once the patient has been put into remission?” Genetic tests or studies on immune cells may be able to offer a clearer prognosis than is currently possible.
Toward better solutions
The stereotype of the lone genius has been exposed as a myth—or at the least the rare exception that proves the rule. Dr. Specks’ and Dr. Fervenza’s research is an example of the truism that two heads are better than one. That’s perhaps the principal reason for scientific collaboration. Says Dr. Specks, “You go to meetings and ideas get tossed around and you discuss, what’s the next question, and you realize that you can better answer it together than in isolation. This is how one thing leads to another.”
Mayo Clinic in particular fosters this kind of collaboration, says Dr. Specks. Its reputation for excellence draws some of the brightest minds in medicine, as well as patients seeking answers when past treatment has failed. Moreover, “clinical care, research and education have always been intertwined and valued. It was understood that we need to excel in all three in order to move the field forward and provide better solutions for patients.”
Moreover, Mayo breaks down barriers between disciplines to improve patient care. That same work environment encourages effective collaboration in research. Of that there’s no better example than Dr. Fervenza and Dr. Specks.
Says Dr. Specks, “We see the same patient together and we discuss this when questions come up. We ask how can we answer these questions together? How can we do studies together? That’s how these things come about. It’s relatively easy at Mayo, probably easier than in many other institutions where the departmental boundaries are much stronger.”
It’s not surprising, perhaps, that the personable Dr. Fervenza would put things somewhat differently—that successful collaborations depend on friendships and social skills. The key? “Not to have a big head,” he says. “Because if you believe that you know everything, then people don’t like to collaborate with you. You need to give and take, and give credit where credit is due.”
- Greg Breining
November 2015